The foundation of a good diabetes care plan is a set of target ranges for blood sugar levels. Blood sugar, or glucose, is sugar in the bloodstream that comes from the foods we eat, particularly from carbohydrates. It’s the primary source of energy for the body. For people who do not have diabetes, the pancreas provides enough insulin to help the body absorb glucose efficiently. But for some people with diabetes, the system doesn’t always work properly. Blood glucose levels must be regulated by taking insulin and diabetes medications and monitored regularly.
Many factors can affect your blood glucose levels, including diet, physical activity, alcohol consumption, illness, and stress. Keeping blood sugar within a normal range is important to balance your mood and energy and avoid long term health problems. When blood sugar is too low (hypoglycemia), or too high (hyperglycemia), serious complications can occur if left untreated. These include nerve damage, heart disease, kidney disease, cognitive problems, and others. The American Diabetes Association (ADA) recommends that adults be screened for diabetes every three years beginning at age 45. For people with other risk factors, screening should begin even earlier. If you experience any of the symptoms commonly associated with diabetes, it’s important to speak with your healthcare provider right away about getting tested.
What are normal blood sugar levels?
If you have type 1 or type 2 diabetes, you may often wonder what your normal blood glucose levels are. Below we’ve outlined general guidelines for most nonpregnant adults with and without diabetes as established by the ADA, but it’s important that you work with your healthcare provider to understand your individual goals. He or she can provide clear guidelines on how your target blood sugar ranges should be set based on your medical history and other considerations. These include things like your age, gender, weight, how long you’ve had diabetes, and whether or not you are pregnant or have a history of gestational diabetes. Other risk factors are also important, including the presence of health conditions like high cholesterol or high blood pressure. All of these factors will help determine if your blood glucose goals should be more stringent or more relaxed.
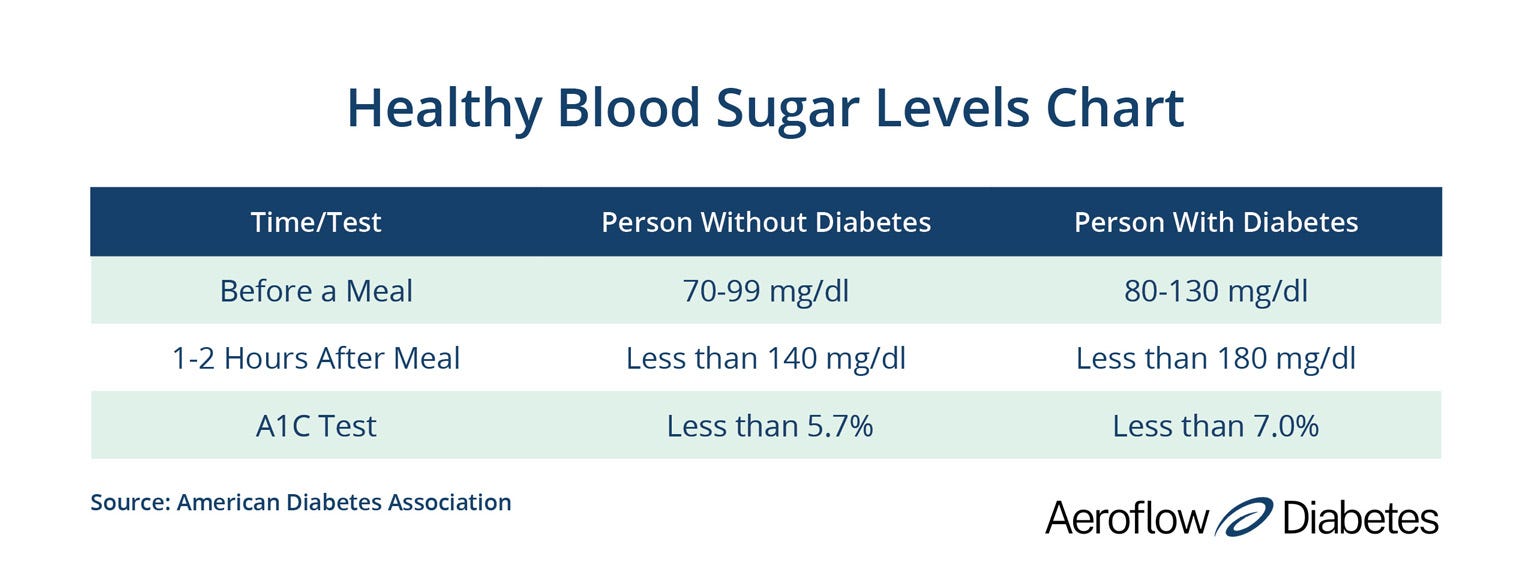
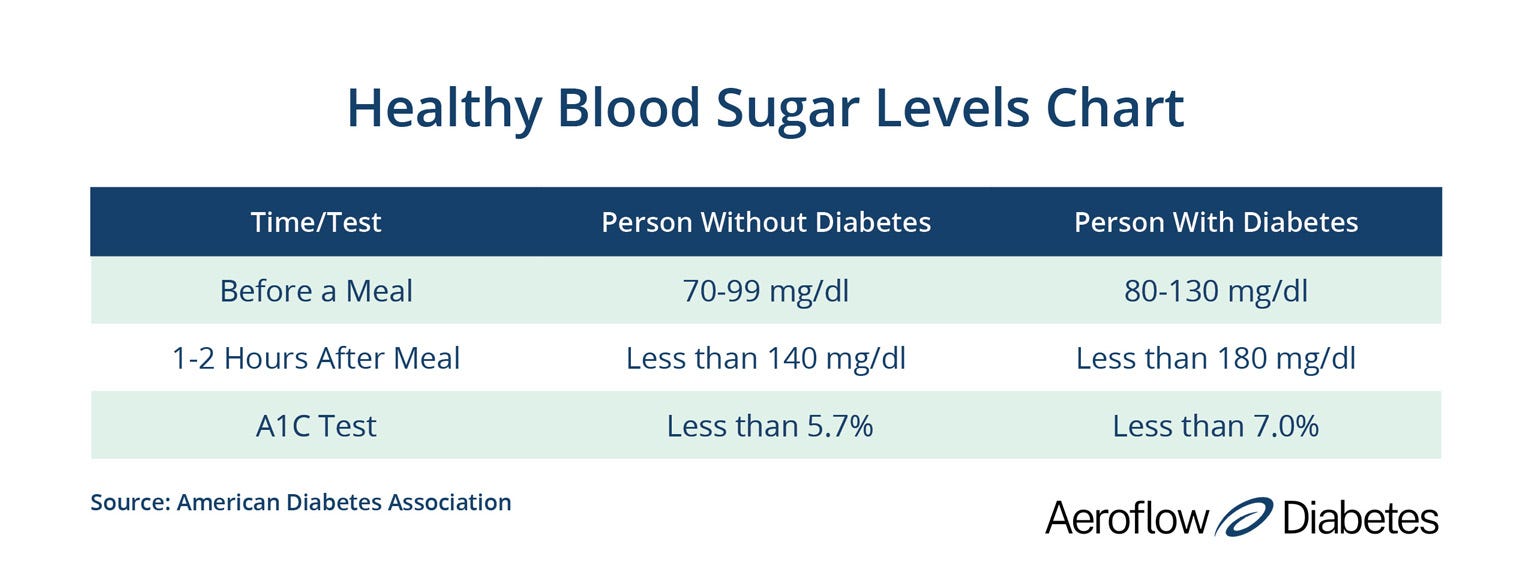
In the United States, we measure blood sugar in milligrams per deciliter, by weight, which is abbreviated as mg/dl. In a person with diabetes, a normal blood sugar reading in the morning upon waking, also called fasting blood sugar, is 80-130 mg/dl. When measured 1-2 hours after a meal, a normal range for someone with diabetes would be less than 180 mg/dl.
How do I check my blood glucose levels?
There are two primary ways to check your blood sugar at home. The first is by using a traditional blood glucose meter. You’ll use a lancet to draw a small amount of blood, usually on the finger tip. The drop of blood is placed onto a test strip that is inserted into the glucose meter to generate a reading. For people who use a glucose meter to check their blood sugar, it can be helpful to use a blood sugar log to keep track of your blood sugar readings and share them with your healthcare provider.
The second way is by using a continuous glucose monitor (CGM). A CGM sensor is placed just beneath the skin’s surface to measure blood glucose continuously and transmit readings every few minutes, so there’s no need for periodic finger stick tests.


Always follow the diabetes treatment plan your healthcare provider has established, including the recommended way to monitor your blood glucose levels daily. If you take insulin, are pregnant, or have erratic blood sugar levels, you may benefit from checking several times per day, as directed by your doctor.
Some CGM devices can be set to alert you when the amount of glucose in your blood is too high or too low. For diabetics who don’t experience typical symptoms associated with high or low blood sugar, these devices can help prevent severe hypoglycemia and hyperglycemia episodes. CGM devices are covered by insurance for people who need frequent adjustments to their insulin doses. Be sure to speak with your doctor to determine whether you would be eligible for insurance coverage.
What is the A1C test?
The A1C test, also called the hemoglobin A1C test or hbA1C test, is a simple yet powerful blood test performed by your endocrinologist. Rather than indicating your blood sugar levels at one moment in time, the A1C test provides a ‘big picture’ view. It gives you your average blood sugar level over the past few months. The A1C test can be used to diagnose prediabetes. While people with prediabetes are at higher risk for developing type 2 diabetes, they still have an opportunity to prevent it. Weight loss and other lifestyle changes can help.
The A1C test also helps people who have already been diagnosed understand how well they are meeting their individual blood sugar goals. Typically, people with diabetes take an A1C test 2-4 times per year. The A1C goal for many adults with diabetes is 7% or less.
Your doctor can help interpret your test results and develop an appropriate treatment plan. Your individualized plan could include recommendations for physical activity, weight loss or other lifestyle changes that can help prevent diabetes complications. You may also be assigned to a diabetes education program or glucose awareness training to learn how to eat the right foods that won’t spike your blood sugar, control carbs, and safely lower high blood sugar levels.
References
Diabetes Symptoms, Centers for Disease Control and Prevention
The Big Picture: Checking Your Blood Sugar, American Diabetes Association (ADA)
Information provided on the Aeroflow Diabetes blog is not intended as a substitute to medical advice or care. Aeroflow Diabetes recommends consulting a doctor if you are experiencing medical issues or concerns.






