Key Takeaways:
- Drink water and take a short walk to help flush excess glucose from your system and lower blood sugar quickly in non-emergency situations.
-
Follow your doctor’s correction dose plan carefully—fast-acting insulin or prescribed medications can help bring glucose levels down safely.
-
Use a CGM to track trends and prevent spikes, and consider pairing it with a diabetes management program for long-term glucose control.

EMERGENCY MEDICAL WARNING: When to Call 911
This article is for managing non-emergency high blood sugar. If your blood sugar is extremely high or you are experiencing the following symptoms, it could be a sign of a life-threatening condition like Diabetic Ketoacidosis (DKA) or Hyperosmolar Hyperglycemic Syndrome (HHS).
Call 911 or go to the nearest emergency room immediately if you have high blood sugar accompanied by any of these symptoms:
-
Fruity-smelling breath
-
Nausea and vomiting
-
Deep, rapid breathing or shortness of breath
-
Extreme drowsiness, disorientation, or confusion
-
High levels of ketones detected in your urine
-
Giving insulin dosage without improvement after 1 hour
Do not try to manage these symptoms at home. Seek immediate medical care.
First Steps to Lower Blood Sugar Immediately
Seeing a high number on your glucose meter can be stressful, but in many cases, you can take steps at home to safely lower it. When you experience hyperglycemia (high blood sugar), it means there is too much glucose, a type of sugar, in your bloodstream. For people with diabetes, this can happen when the body doesn't have enough insulin or can't use insulin effectively.
In a non-emergency situation, the fastest ways to help lower your blood sugar are to
-
Drink few glass of water.
-
Take a short walk.
-
Follow your doctor's prescribed plan for correction doses of medication or insulin.
This guide will walk you through each of these steps, explain why they work, and help you understand how to prevent future spikes.
What Is Considered High Blood Sugar (Hyperglycemia)?
While your blood sugar targets should be set by your doctor, the American Diabetes Association (ADA) provides general guidelines for most adults with diabetes.
-
Fasting Blood Sugar (before a meal): 80–130 mg/dL
-
Post-Prandial Blood Sugar (1-2 hours after a meal): Below 180 mg/dL
Hyperglycemia occurs when your blood sugar rises above these targets. It's important to know that a single high reading is not always a cause for alarm, but it is a signal to pay attention and take action.
Levels of concern:
-
Mildly High: A reading slightly above your target range.
-
Persistent Highs (above 180-200 mg/dL): If your blood sugar remains high for several hours, it's time to use the management steps outlined below.
Very High (above 250 mg/dL): At this level, it is important to check your urine for ketones. The combination of very high blood sugar and ketones can be a precursor to DKA and requires a call to your healthcare team for guidance.
Common Symptoms of High Blood Sugar
Sometimes you can feel the effects of hyperglycemia before you even check your meter. Recognizing these symptoms is the first step toward taking action.
Early Symptoms:
-
Increased thirst and a dry mouth
-
Frequent urination
-
Fatigue or feeling more tired than usual
-
Blurred vision
-
Headache
More Severe Symptoms:
-
Fruity-smelling breath
-
Nausea, vomiting, or stomach pain
-
Shortness of breath
-
Confusion or difficulty concentrating
If you are experiencing any of the more severe symptoms, please refer back to the emergency warning at the top of this page and contact your doctor or seek immediate medical care.
Drink Water to Rehydrate and Flush Your System
This is the simplest and safest first step you can take. High blood sugar makes your body lose fluid, leading to dehydration, which can make your blood sugar concentration even higher.
-
What to do: Drink a full, 8-ounce glass of plain water right away. Continue sipping more water over the next hour.
-
Why it works: When your blood sugar is high, your kidneys go into overdrive trying to flush the excess glucose out of your system through urine. Drinking water helps your kidneys perform this function more efficiently and rehydrates your body, helping to dilute the glucose in your bloodstream.
Important Safety Note: Stick to plain water. Avoid juices, sodas (even diet ones), or sports drinks, as they can contain sugars or other ingredients that may raise your blood sugar.
Take a Short Walk
Physical activity is another fast and effective way to lower your blood sugar.
-
What to do: Engage in 10-15 minutes of light-to-moderate physical activity, such as a brisk walk, a gentle bike ride, or some bodyweight exercises.
-
Why it works: When you exercise, your muscles need energy. To get it, they pull glucose from your bloodstream, which directly lowers your circulating blood sugar levels. Regular exercise also helps improve your body’s insulin sensitivity over time.
-
Important Safety Note: Do not exercise if you have checked your urine and ketones are present. If you have type 1 diabetes, exercising with high ketone levels can actually cause your blood sugar to rise even higher.
Follow Your Doctor's Plan for Correction Doses
If you use medication or insulin for diabetes, your doctor has likely provided you with a plan for what to do when your blood sugar is high. Now is the time to refer to that plan.
-
What to do: Review the specific instructions from your healthcare provider for a "correction dose." This may involve taking a dose of fast-acting insulin (like lispro/Humalog or aspart/Novolog) or another prescribed medication.
-
Why it works: Fast-acting insulin or certain oral medications are designed to quickly counteract high blood sugar levels by helping your body absorb glucose from the blood into the cells.
-
Important Safety Note: Never take more medication or insulin than prescribed. This article cannot provide dosage advice. Your "correction factor" is unique to you. Taking an incorrect dose can be dangerous and lead to hypoglycemia (low blood sugar). If you are unsure what to do, call your doctor or endocrinologist's office.


What to Eat to Help Stabilize Your Blood Sugar
While no food will magically lower your blood sugar instantly, choosing the right snack can help stabilize your levels and prevent them from climbing even higher while you wait for your body to recover.
-
What to do: If you need to eat, choose a small snack that is high in protein, fiber, or healthy fats, but low in carbohydrates. Examples include a handful of almonds, a hard-boiled egg, or a piece of string cheese.
-
Why it works: Unlike carbohydrates, protein and fat have a minimal immediate impact on blood sugar levels. This can help satisfy hunger without adding more glucose to your system.
Important Safety Note: Stay away from carb-heavy snacks like chips, cereal, fruit, or sweets until your blood sugar has returned to your target range.
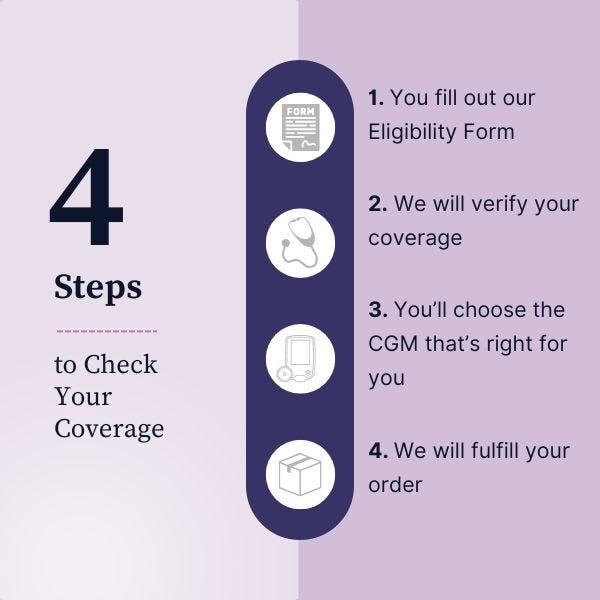
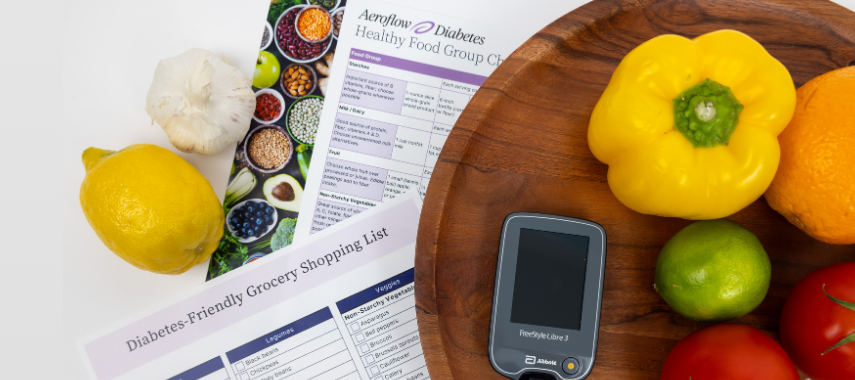
Gain Control with Technology and Support from Aeroflow
At Aeroflow Diabetes, we make it easy to get the supplies and support you need. A Continuous Glucose Monitor (CGM) is a game-changing tool that tracks your glucose levels 24/7 without the need for constant fingersticks. It alerts you when you’re trending high so you can take action early, giving you more control day-to-day.
A CGM is even more powerful when paired with expert guidance. That's why Aeroflow Diabetes also offers a Diabetes Management Program, providing personalized education on diet, exercise, and how to use your device data to achieve your long-term health goals.
To see if you qualify for a CGM through your insurance and learn more about our support programs, simply fill out our secure Eligibility Form. Our team will handle the insurance paperwork and, if you're approved, ship your supplies directly to your home.
Disclaimer
Information provided on the Aeroflow Diabetes blog is not intended as a substitute to medical advice or care. Aeroflow Diabetes recommends consulting a doctor if you are experiencing medical issues or concerns.