Key Takeaways:
- Diabetes in children is on the rise, with both type 1 and type 2 becoming increasingly common and often showing symptoms within days to a week.
-
Early signs include excessive thirst, fatigue, weight loss, frequent urination, and blurred vision—prompt testing is essential for diagnosis.
-
Modern tools like continuous glucose monitors (CGMs) and insulin delivery systems can greatly improve diabetes management in children.

According to the Centers for Disease Control (CDC), diabetes is a chronic health condition that affects the body’s ability to convert sugar into energy. When a child has diabetes, their body either doesn’t make enough insulin or can’t use the insulin it makes as well as it should. This leads to high levels of sugar (glucose) in the bloodstream. Both of the main types of diabetes, type 1 and type 2, can affect children and adolescents.
Recent CDC data highlights a growing concern: from 2001 to 2017, the number of people under age 20 living with type 1 diabetes increased by 45%, and the number living with type 2 diabetes grew by 95%. Understanding the differences, symptoms, and modern treatments is key for any parent.
Juvenile Diabetes
Formerly known as juvenile diabetes, type 1 diabetes is the most common form in children, accounting for the majority of diagnoses. It is an autoimmune disorder where the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas.
The exact cause of type 1 diabetes is unknown, but it is believed to involve a combination of genetic predisposition and environmental triggers. It is not caused by diet or lifestyle choices. Without insulin, glucose in the blood cannot be converted into energy, causing it to build up in the blood (leading to high sugar levels). Children diagnosed with type 1 diabetes will typically require lifelong insulin therapy.
Type 2 Diabetes
Type 2 diabetes is being diagnosed more frequently in children and teens. In this instance, the body displays insulin resistance, or difficulty using insulin properly. Initially, the pancreas produces more insulin to compensate for this difficulty, but eventually, it can’t keep up, and high blood glucose follows.
While there is a genetic component to type 2 diabetes, the risk of this condition is significantly increased by lifestyle factors. Being overweight or obese is a primary risk factor. Your child’s doctor may recommend lifestyle changes, including a healthy diet and regular exercise to boost insulin sensitivity. In some cases, medication or insulin therapy may be necessary.
Symptoms of Type 1 & 2 Diabetes in Children
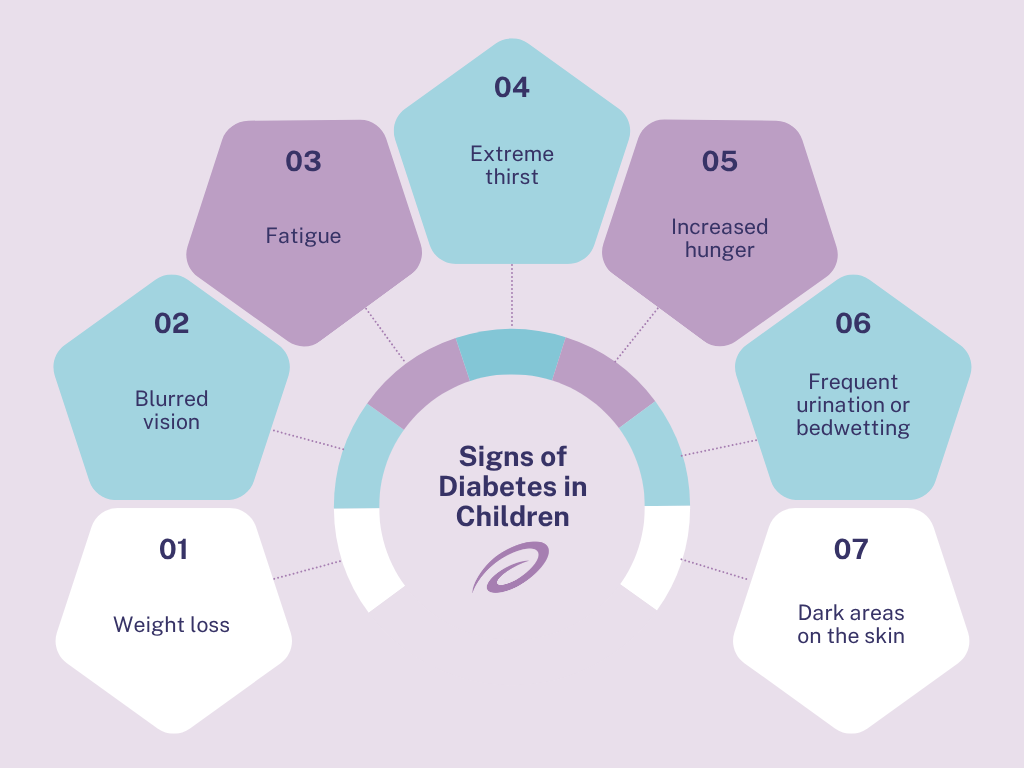
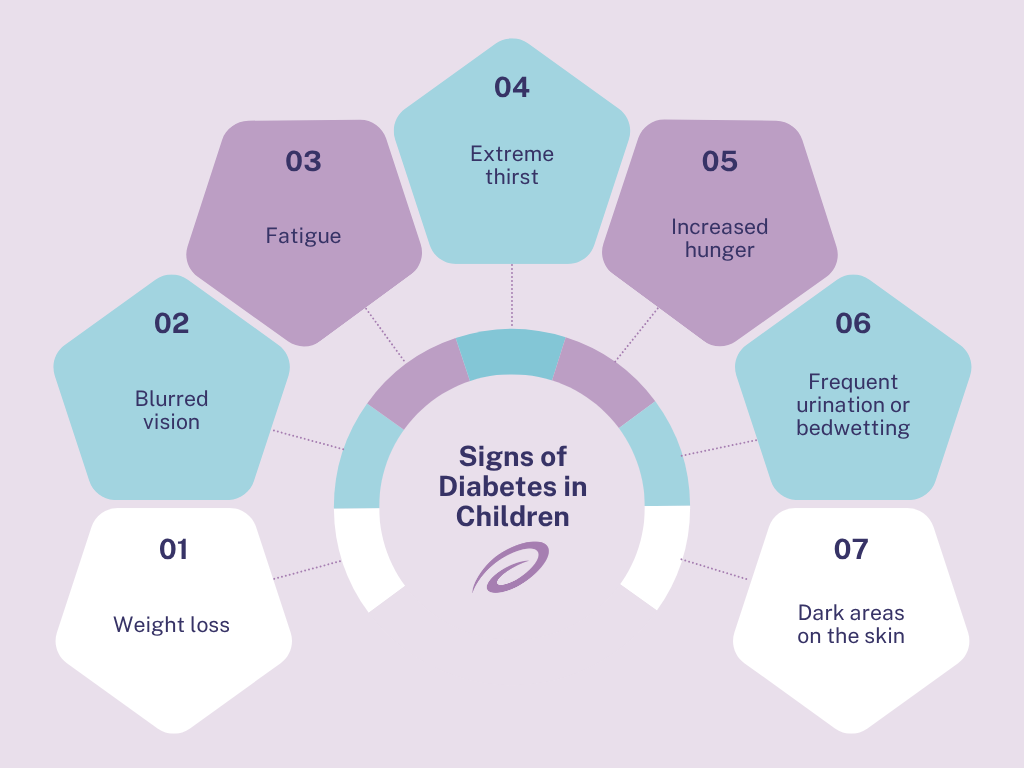
Symptoms associated with diabetes can start to show in only a few days to a week, warning signs include:
-
Weight loss: Weight loss is more common in children diagnosed with type 1 diabetes.
-
Blurred vision: When glucose levels in the blood get too high, fluid in the eyes can be affected, making it difficult to focus.
-
Fatigue: High blood sugar levels can make a child feel tired, lethargic, and irritable.
-
Extreme thirst: Liquid is pulled from tissues in the body when blood sugar levels are too high, causing feelings of thirst.
-
Increased hunger: Without enough insulin to help the body use glucose, muscles and organs are low on energy, triggering intense hunger sensations.
-
Frequent urination or bedwetting: Because the body is pulling fluid from tissues and there is increased thirst and fluid intake, your child may feel the need to urinate more than usual.
-
Dark areas on the skin: Children with type 2 diabetes may develop dark spots on their skin, particularly in the armpits and around the neck.
Undiagnosed diabetes can lead to a serious condition known as diabetic ketoacidosis (DKA). When the body cannot utilize the sugar in the blood, it’s forced to break down fat for fuel causing high levels of blood acids, known as ketones, to build up in the bloodstream. Diabetic ketoacidosis is a life-threatening condition and can be diagnosed with a simple blood or urine test. Symptoms of DKA include many of the above symptoms in addition to:
-
Shortness of breath
-
Confusion
-
Abdominal pain
-
Nausea and vomiting
-
Fruity smelling breath
-
Dry mouth
Testing for Diabetes in Children
If your child is experiencing symptoms of diabetes, it is important to speak with a healthcare provider as soon as possible. Diagnosis is straightforward and typically involves one or more of the following tests:
-
Random Blood Sugar Test: A blood sample is taken at a random time. According to the American Diabetes Association (ADA), a blood sugar level of 200 mg/dL or higher suggests diabetes.
-
A1C Test: This blood test indicates the average blood sugar level for the past two to three months. An A1C level of 6.5% or higher on two separate tests indicates diabetes.
-
Fasting Blood Sugar Test: A blood sample is taken after an overnight fast.
-
Oral Glucose Tolerance Test (OGTT): This test measures blood sugar before and after drinking a specialized sweet drink.
According to the American Diabetes Association, blood sugar levels 200 mg/dl or higher indicate diabetes. Even if your child shows mild symptoms, it may be beneficial to get tested as almost all children who develop type 2 diabetes have prediabetes. Children that have blood sugar readings that fall above the normal range but are still below 200 mg/dl are considered prediabetic.
Diabetes Management and Treatment
Your child’s doctor will be able to recommend a treatment plan specific to your child’s needs. Depending on the type and severity, treatment options may include:
-
Monitoring and counting carbohydrates
-
A healthy diet
-
Physical activity
-
Blood sugar monitoring
-
Insulin therapy
-
Oral medications
Advanced Blood Sugar Monitoring
Children diagnosed with type 1 diabetes will be required to test their blood sugar multiple times a day. While traditional finger-stick tests are still used, continuous glucose monitors are now considered the standard of care.
A continuous glucose monitor (CGM) consists of a small sensor placed under the skin and a receiver, or mobile device app, that receives and translates the data. CGM’s can alert you if your child’s glucose is trending too high or too low, providing peace of mind and allowing for proactive management. Most CGMs, including the Dexcom G7 and Abbott FreeStyle Libre 3 and 3Plus, integrate with insulin pumps to create automated insulin delivery (AID). These smart systems can automatically adjust insulin delivery based on CGM readings, helping to keep blood sugar levels more stable.
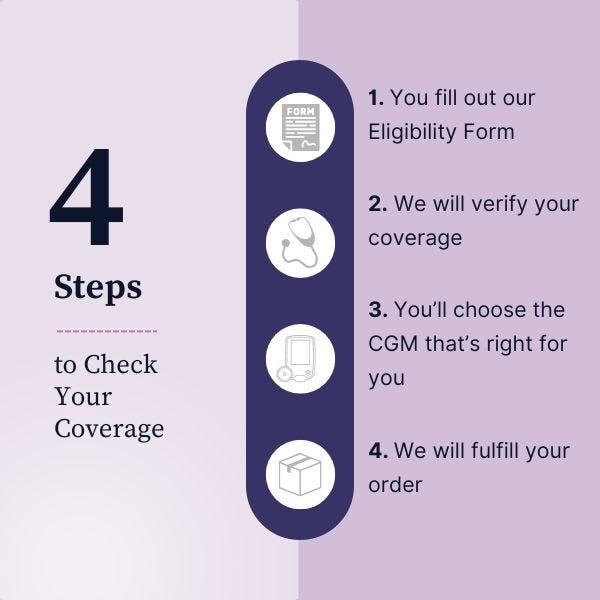
Speak with your healthcare provider to see if a CGM or AID system is right for your child. To see if your child is eligible for a continuous glucose monitor, fill out our quick form to check your child’s eligibility.
Disclaimer
Information provided on the Aeroflow Diabetes blog is not intended as a substitute to medical advice or care. Aeroflow Diabetes recommends consulting a doctor if you are experiencing medical issues or concerns.
References
Centers for Disease Control and Prevention. (2024). National Diabetes Statistics Report.
Centers for Disease Control and Prevention. (2024). Diabetes in Kids and Teens.
American Diabetes Association. (2025). Standards of Care in Diabetes—2025. Diabetes Care, 48(Supplement 1).
Mayo Clinic. (2024). Type 1 diabetes in children.
Mayo Clinic. (2024). Type 2 diabetes in children.