Urinary tract infections can be a pain to manage, especially if you get them more often due to diabetes. Learn how to identify urinary tract infection symptoms and get 4 prevention tips from our Diabetes Expert.
What Is a UTI?
A UTI is a urinary tract infection. This infection occurs in the urinary system in either the kidney, bladder, ureters, or urethra. It’s common for people to develop UTIs in their bladder or urethra, but they can occur in the kidneys.
Why Do People With Diabetes Get UTIs?
People with diabetes have a higher risk of all infections, and UTIs are the most common.
High blood sugars are associated with a weakened immune system, and when your immune system is weakened, it’s easier for your body to develop an infection like a UTI.
UTIs occur when bacteria enter through your urethra and get into your urinary system, causing an infection. It’s easier for these bacteria to infect your body when your immune system is weakened, like those with high blood sugars have.
In addition, it is felt that higher levels of sugar in the urine may cause UTI’s to be more severe in people with diabetes. Diabetic neuropathy— pain and numbness in the legs and feet— can actually affect the bladder and cause incomplete bladder emptying (urinary retention), which creates a favorable environment for bacteria to reproduce and cause infection like UTIs.
According to our experts, UTIs occur in people with diabetes quite frequently. It’s more common in adults regardless of the type of diabetes they have (type 1, type 2, gestational). Pregnancy can increase the risk of UTIs, but people with gestational diabetes are at higher risk than those without.
Symptoms
Typically the symptoms of UTIs in people with diabetes are the same as in people without diabetes, but since UTIs can possibly be more severe in those with diabetes, they may have more severe symptoms that can possibly progress to worse infection, such as pyelonephritis (infection of the kidneys), and even sepsis (infection in the blood stream) if not treated in time.
Typical Symptoms of UTIs:
- Strong urge to urinate.
- Burning when urinating.
- Urinary retention (urinating only a small amount).
- Excessive urination.
- Foul or strong-smelling urine.
- Cloudy-looking urine.
- Pain in the lower back.
- Pain in the pelvic area.
Since UTIs can actually contribute to higher blood sugars, people with diabetes may experience more frequent urination than those without. However, people with diabetic neuropathy affecting the urinary tract may actually have less severe or even no symptoms at all.
Treatment
Fortunately, UTIs are easy to diagnose with a urine specimen and are typically easy to treat with the appropriate antibiotics.
The most important step is early diagnosis and appropriate treatment. A simple urinalysis can be done immediately to identify an infection, so it’s important to have a urinalysis test done at the first sign of UTI symptoms.
A urine culture can then be done which will identify the bacteria responsible for the urinary infection. The lab can then test the bacteria against multiple antibiotics to ensure the correct antibiotic is used for treatment.
Home remedies such as AZO may help reduce symptoms but do not actually treat the infection (which typically requires an antibiotic).
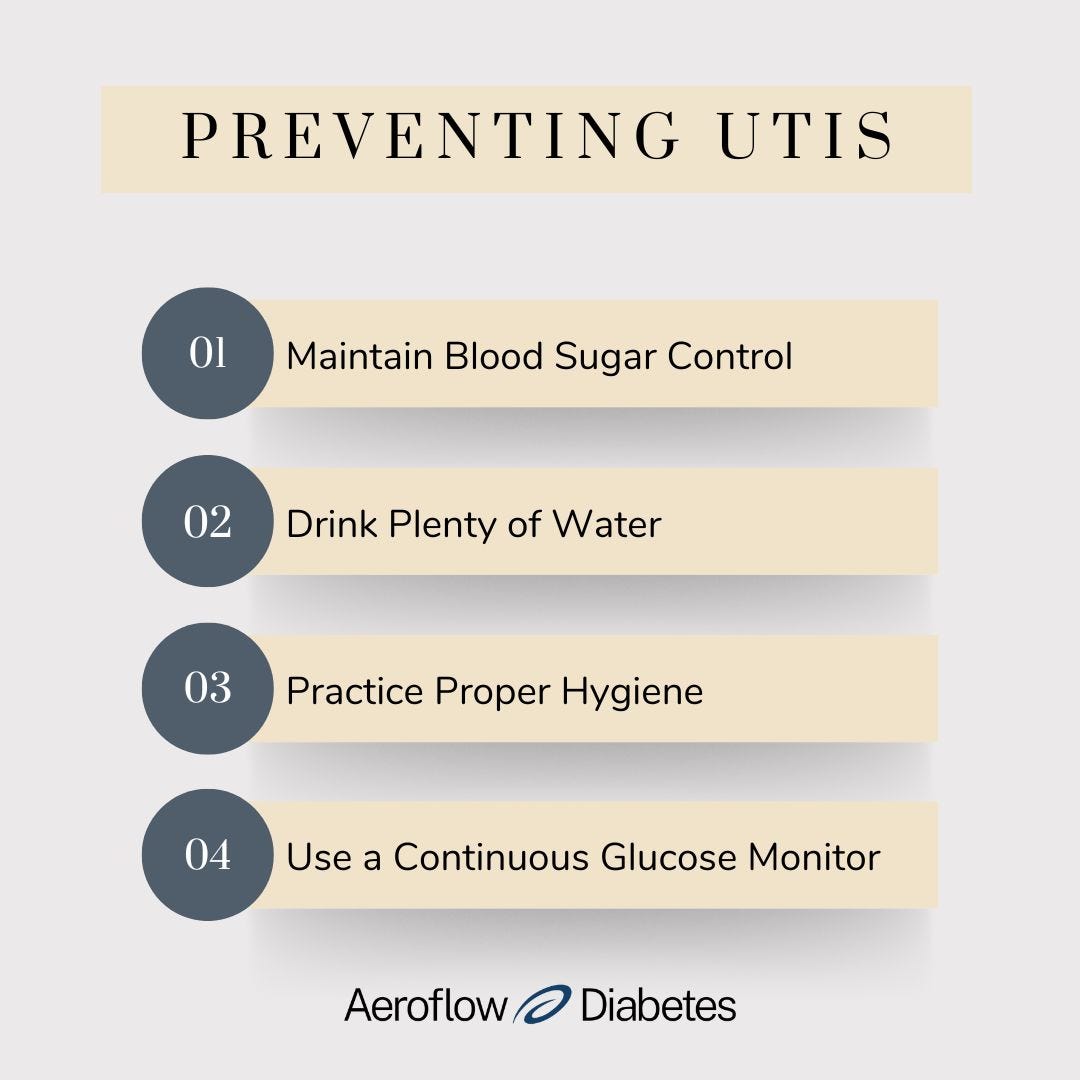
Prevention
1. Maintain blood sugar control. This is an important first step in preventing UTIs. To manage your blood sugar levels, eat a healthy diet, get exercise, and maintain a healthy weight.
2. Drink plenty of water. Staying hydrated will help maintain urine output which can clear out bacteria and keep your urinary system functioning properly. It can also help lower the acidity of your urine (dehydration causes concentrated urine) which lessens the number of times you need to void your bladder.
3. Practice proper hygiene. For women, it is important to practice good hygiene since bacteria can enter the urinary tract much easier than in men. Shower or bathe 2-3 times a week and use mild soaps.


4. Use a Continuous Glucose Monitor. If you have type 1 diabetes or type 2 diabetes, you may qualify to receive a Continuous Glucose Monitor (CGM) through insurance. CGMs are great diabetes management tools that make measuring your blood glucose levels easy without painful finger pricks. They also prevent episodes of low blood sugar and high blood sugar levels by warning you when levels are too high or low.
If you’d like to see if you qualify for a low-cost CGM through insurance, fill out our Eligibility Form. It takes less than 5 minutes and after submitting the form, one of our Diabetes Experts will reach out to confirm your eligibility. Then, your CGM supplies will be shipped to your door every month and you’ll get reminded when it’s time to refill your items.
Information provided on the Aeroflow Diabetes website is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to diabetes care.