Key Takeaways:
- Both high (hyperglycemia) and low (hypoglycemia) blood sugar levels can cause excessive hunger in people with diabetes, but they require different treatments—either insulin or fast-acting carbs.
- Avoiding blood sugar fluctuations by eating balanced meals, including a healthy breakfast, and working with a healthcare team can help prevent excessive hunger.
- It’s important to differentiate between true hunger and emotional cravings, as cravings can lead to overeating and difficulty controlling blood sugar levels.
For those living with diabetes, hunger can be more than just a craving, but blood sugar imbalances as well. Both high and low blood sugar levels can trigger excessive hunger, but the causes and management of each vary. Monitoring these fluctuations is important to help prevent unnecessary hunger and maintain proper blood sugar levels.
Use this article to learn how diabetes can impact hunger, the importance of recognizing blood sugar changes, and strategies to control hunger while keeping diabetes in check.
Hunger and Hyperglycemia
Eating food increases blood sugar levels, and in those without diabetes, this triggers the pancreas to produce insulin. Insulin helps the cells in the body use that blood sugar for energy or store it away for later. In people with diabetes, the pancreas may make too little insulin alongside insulin resistance or may not make any insulin at all.This means that when you eat, your blood sugar levels go up, but the insulin produced by the pancreas is not sufficient to help allow your cells to access the blood sugar as fuel for your body. Glucose builds up in the blood, but since your cells can’t access it, your body still feels hungry. Having high blood glucose levels is a condition called hyperglycemia.
With hyperglycemia, simply eating more may not help to curb your hunger pangs and can continue to drive your blood glucose levels higher. This in turn leads to an even stronger feeling of hunger.
For people with type 1 and type 2 diabetes, it’s important to learn the symptoms of hyperglycemia and how it can be prevented. Managing stress and eating a healthy diet with the right kinds of carbohydrates can help keep high blood sugar levels at bay. Diabetes medications may be recommended for people with type 2 diabetes, and insulin is needed to control high blood glucose for those with type 1 diabetes. A continuous glucose monitor (CGM) may also be a helpful tool to continuously monitor blood glucose levels in real-time.
Hunger and Hypoglycemia
Excess hunger can also be caused by abnormally low blood sugar levels, a condition called hypoglycemia. According to the American Diabetes Association, blood sugar is typically considered low at less than 70mg/dL.
For people with diabetes, skipping a meal can lower blood sugar levels to well below the target range. Other causes could be excessive exercise, taking too much insulin, or eating highly refined carbs, which can cause the blood sugar levels to spike and then fall quickly.
Unlike hyperglycemia, hypoglycemia can often be treated by eating fast-acting carbohydrates. It can take some practice to learn which foods are best to eat to raise your blood sugar to a safe level without overeating.
It’s also important to work with your healthcare team to avoid hypoglycemic events in the future. Your primary care provider or endocrinologist can determine your target blood sugar ranges. A dietitian can help adjust your meal plan to give you better blood sugar control.
CGMs and Monitoring Blood Sugar Levels
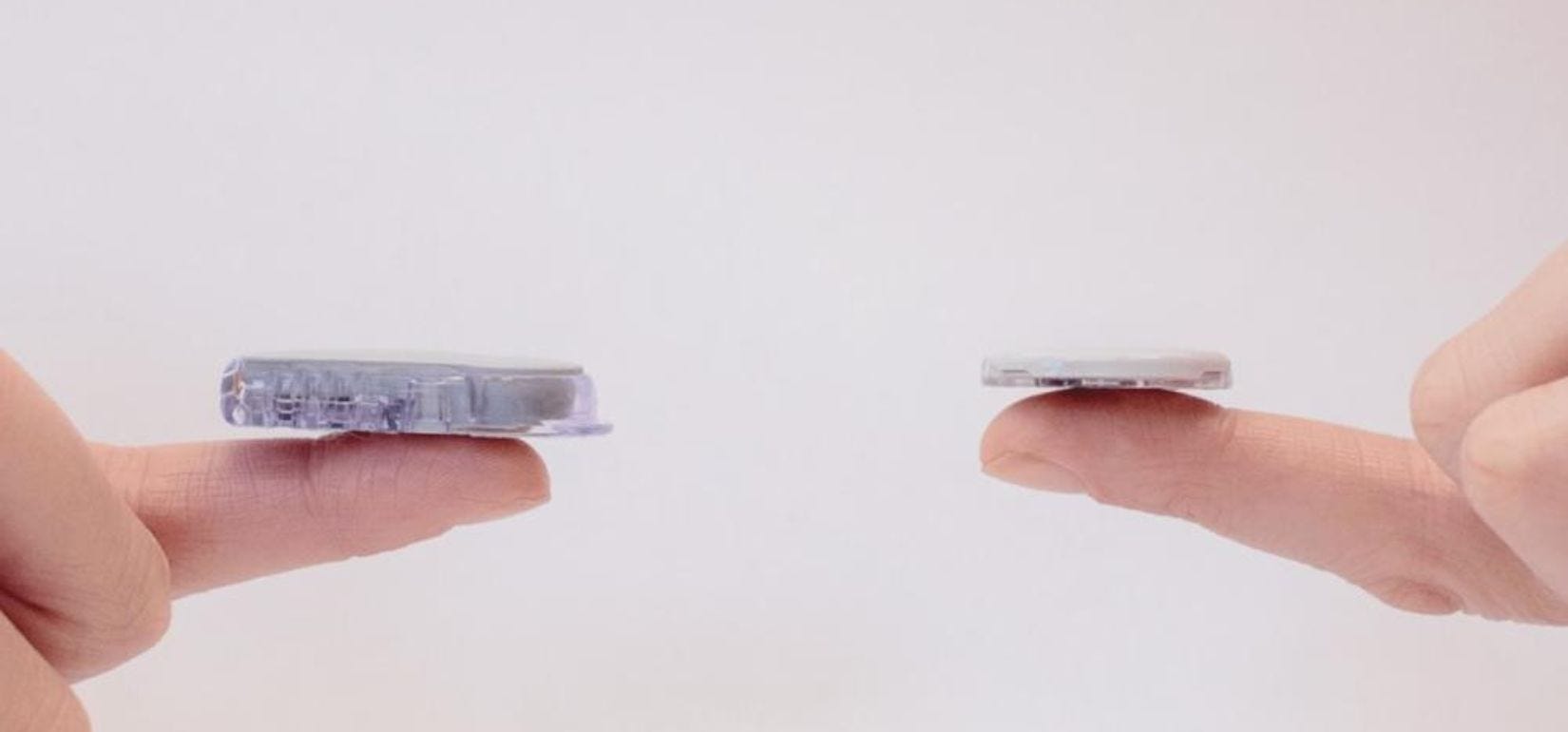
If you experience excessive hunger, it’s critical to check your blood sugar levels so that you know if you are dealing with hyperglycemia or hypoglycemia. Thankfully, diabetes technology has advanced, and you can now use painless CGMs to receive accurate glucose data.
CGMs are wearable devices that monitor your blood glucose levels painlessly, and in real-time. Diabetes management can sometimes be tedious, but glucose monitoring is the most crucial aspect of diabetes care. With a CGM, you can instantly know when to administer the proper treatment to either raise or lower your blood sugar safely. Find out if you qualify for your own CGM by filling out our quick Eligibility Form.
Curbing Hunger with Diabetes


The best way to manage excessive hunger with diabetes is to work to prevent it before it starts. This means avoiding dramatic swings in your blood sugar levels. Refer to this list we’ve put together of nutrient-rich foods with low glycemic scores that won’t spike your blood sugar and will help you feel full. Staying within your target range consistently will ensure that your cells get the energy they need so you won’t feel so empty. This will also help to reduce the risk for diabetes complications. Here are a few ways to help keep your blood sugar levels in check:
1. Distinguish Real Hunger from Food Cravings.
We can all experience cravings from time to time, diabetes or not. Food cravings tend to emerge suddenly, and can sometimes be curbed by something as simple as a temporary distraction. They are different from true hunger in that they are typically focused on a specific type of food.
It may be that we see a sweet treat that reminds us of a positive experience or place. Or it may be a habit to indulge in comfort food after a stressful event to calm the nerves. For people with diabetes or those on restrictive diets, it may be that they aren’t allowing themselves enough of the foods they enjoy in their daily meal plan.
Whatever the cause, food cravings can lead to overeating and eventually weight gain, which can make diabetes harder to control. It’s important to speak with a certified diabetes care and education specialist (CDCES) or dietitian to develop a meal plan that works to control blood sugar levels without being too restrictive. If you have diabetes and feel an intense food craving coming on, it’s a good idea to check your blood sugar to see if you are experiencing high or low blood sugar.
2. Eat a Balanced Breakfast.
Eating a balanced breakfast is crucial when you’re managing diabetes. A breakfast that is rich in protein and fiber with a low to moderate amount of carbohydrates and healthy fats is the goal. This will help set a good foundation for healthy blood sugar levels throughout the day. Steer clear of highly refined carbohydrates like cereals and baked goods, which can cause a quick spike in blood sugar followed by a crash.
Part of the way we are satisfied when we eat has to do with how the food looks and smells. Take time to really savor and enjoy your food; this goes for breakfast as well as all other meals and snacks. If you get stuck in a breakfast rut, try and shake things up so you don’t get bored with your meal. Try these diabetes-friendly breakfast ideas from the American Diabetes Association.
3. Keep Your House Tempt-Free.
It’s easier to avoid trigger foods that can spike your blood sugar levels if they aren’t in your fridge or cupboard. Take time to clear out the problem foods and replace them with healthy alternatives. Don’t forget about your workplace. You may be surprised to find plenty of healthy snack options when you’re looking to satisfy a certain craving. Unsalted or lightly salted nuts or popcorn can take the place of chips, for example. The popularity of healthy snacks, whole foods based snacks, or minimally processed snacks in recent years means that you can often even find packaged foods that are diabetes-friendly. Reading the nutrition label can ensure you're making choices in line with your goals.
Taking this step not only limits exposure to foods that can end up causing more hunger in the long run, it can help create a certain peace of mind if you know you won’t be faced with temptation throughout the day.
Take a Nutrition Class with Aeroflow Diabetes
Did you know Aeroflow Diabetes goes beyond helping you manage your blood glucose levels with CGMs? Medical Nutrition Therapy (MNT) is an evidence-based program that integrates with medical management of diabetes. MNT offers personalized diabetes support with registered dietitians who will help improve your glycemic control and promote weight loss, while reducing cardiovascular risk factors and diabetes symptoms.
This insurance-covered program provides a great opportunity to improve your health and well-being—right from the comfort of your own home. Take control of your diabetes management in an even more in depth way, with preventative care and lasting results. Call 866-902-1623 or email nutrition@aeroflowinc.com to sign up for a class today, or to find out more about the different types of MNT classes offered!


Get CGMs Through Insurance
Find out if you or a loved one qualifies for a CGM through your insurance by completing our quick and secure Eligibility Form.
The process is simple, and we guarantee your information will remain confidential. Once submitted, we'll contact you shortly to let you know your eligibility status.
If you're eligible, you can select from a range of high-quality CGMs that are covered by insurance, available right from your phone or computer. Depending on your insurance plan, options may include:
Don't forget to explore our blog for helpful resources, including answers to common questions about your CGM, managing the ins and outs of type 1 or type 2 diabetes, insurance updates and more!
Aeroflow Diabetes Disclaimer
Information provided on the Aeroflow Diabetes blog is not intended as a substitute to medical advice or care. Aeroflow Diabetes recommends consulting a doctor if you are experiencing medical issues or concerns.