Key Takeaways:
- Continuous Glucose Monitors (CGMs) offer a low-pain, more convenient alternative to traditional finger prick testing by using a small sensor placed just under the skin to measure glucose levels through interstitial fluid.
-
CGMs provide more frequent, real-time glucose data, which can help improve diabetes management decisions and overall health outcomes.
-
CGMs require fewer calibrations and minimal maintenance, with most sensors lasting 10-15 days allowing users to monitor glucose levels even while sleeping, showering, or exercising.

Using a blood glucose meter with a finger stick has long been the most common method for checking blood sugar levels. If you’re one of the 30 million Americans who lives with diabetes, you know that testing your blood sugar can be a tedious process. A lancet is used to prick the finger, and a small sample of blood is collected on a test strip. This sample is inserted into the blood glucose meter, or glucometer, for measurement. This process can be repeated up to four or more times a day.
Is There a Way to Monitor Blood Sugar Without Needles?
The first step in ditching the finger stick test is to speak with your healthcare provider about the possibility of switching to a continuous glucose monitor (CGM).
Your healthcare provider will help determine the best brand for your needs and make sure you are comfortable using your device. Be aware that some CGM systems may require calibration, which means testing your CGM results against the results of, you guessed it, a finger stick test. But this still adds up to a lot less finger pricking and a lot more time back in your day.
What Is a CGM?
A CGM is a sensor-based device that provides real-time glucose readings day and night, without requiring fingersticks.
Relying on interstitial fluid, not a blood sample, a small sensor is placed just under the skin with a needle, which retracts back into the applicator and does not stay in the arm. It is still a penetration of the skin, but it is a very shallow puncture and a CGM needs to be applied and replaced only every 10-15 days. It is usually placed on the back of the upper arm or on the abdomen, continuously monitoring and reporting your glucose levels.
Held in place with an adhesive patch, you can wear a CGM system while sleeping, showering, or exercising. While it’s sometimes confused with an insulin pump, a CGM is designed to monitor and report glucose measurements, not administer insulin.


How Do CGMs Work?
A small sensor is placed just under the skin to collect glucose data. The wearable sensor is attached to a transmitter on top of the skin, which transmits the collected glucose data to the dedicated reader, receiver, or to a smartphone app.
How Accurate Are CGMs?
CGMs are highly accurate and reliable for tracking glucose trends in real-time. FDA-approved CGMs, like Dexcom and FreeStyle Libre Systems, have been clinically proven to offer accuracy levels sufficient for making treatment decisions without a finger stick.
What Are the Benefits of CGMs?
In addition to being a time-consuming process, finger sticking can be painful, which in some cases can lead to avoidance of the process. Testing less often means less awareness of blood sugar levels, making CGMs the preferred tool.
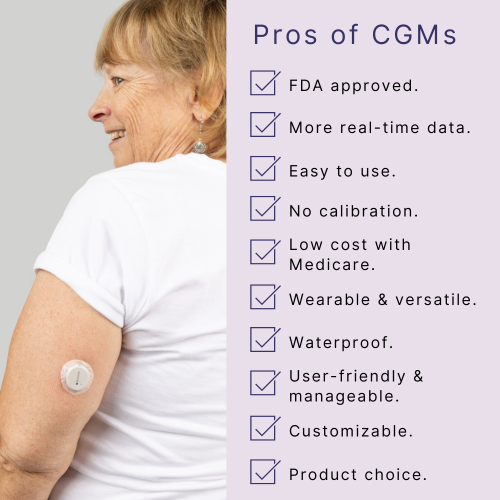
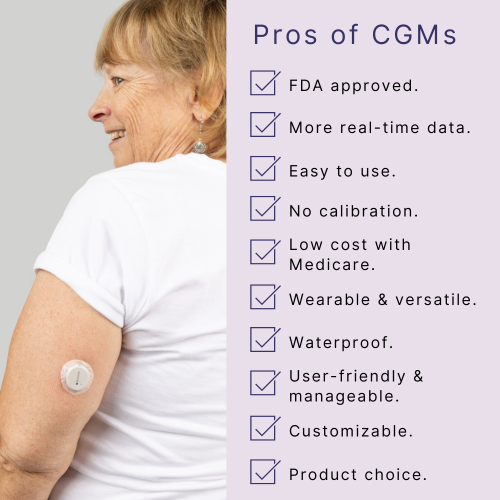
Among several other benefits, CGMs provide continuous, real-time glucose readings without constant finger sticks—offering a painless, user-friendly, and accurate alternative that’s customizable, waterproof, and often low-cost through Medicare, Medicaid, and most commercial insurances, making diabetes management easier for both users and caregivers.
How Much Do CGMs Cost?
The price of CGM varies depending on the brand you get and the features included. Some products are made to be used with a dedicated reader, while some can be used in conjunction with a smart device. There are various alerts and other options that can be set as well. Like everything else in the technology space, extra bells and whistles are always available.
There are a few ways you may be able to receive a CGM at little to no cost.
Are CGMs Covered By Insurance?
If you have a diabetes diagnosis, use insulin and, require frequent adjustments to your dosage, or suffer hypoglycemic episodes, private insurance, Medicare or Medicaid may cover the cost of a CGM system. There are different levels of coverage available, depending on your insurance plan, and in addition to a prescription, your plan may require prior authorization.
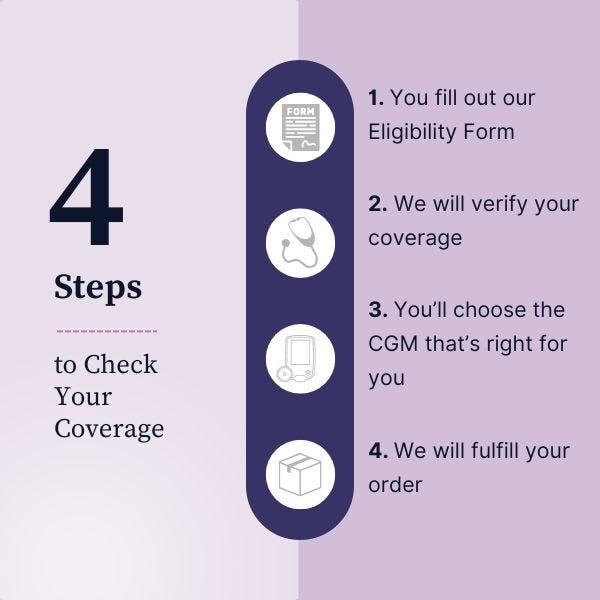
Aeroflow Diabetes is here to help when it comes to navigating your plan requirements and we’ll even coordinate with your healthcare provider to make sure your device is covered if you’re eligible.
What’s the Best Way to Monitor Blood Sugar?
As you no doubt know, blood sugar testing is an important tool in the arsenal for individuals with diabetes. Doctors will recommend testing your blood sugar levels anywhere from 4-10 times a day, usually when you wake up, before and after meals and snacks, before you exercise, before bedtime and more often when you’re ill.
Those with type 2 diabetes who don’t take insulin may not need to test blood glucose daily. If you find yourself with sore, calloused fingers, you may talk with your doctor about alternatives to the finger stick test, and you would need to make sure that your blood glucose meter has clear instructions on alternative test sites as well.
For those who may need blood glucose monitoring during the night or have low blood sugar while they sleep or with few symptoms, it’s worth it to have a conversation with your healthcare provider to see whether CGM is right for you.
Do I Still Have to Fingerstick Check While Using a CGM?
In most cases, fingerstick tests are rarely needed once you're using a CGM. Now, advances in diabetes care and technology have provided new, pain-free options to monitor glucose levels.
These newer glucose monitoring devices are increasingly prescribed by healthcare providers as an alternative to the traditional blood sugar monitors you may be familiar with. Not only do they eliminate the painful finger stick, but they provide more glucose readings throughout the day, and offer a wealth of information regarding how eating, drinking, exercising, and taking medications affect your sugar. More readings and more data means more informed diabetes management decisions.
Disclaimer
Information provided on the Aeroflow Diabetes blog is not intended as a substitute to medical advice or care. Aeroflow Diabetes recommends consulting a doctor if you are experiencing medical issues or concerns.